- Home
- News Room
- Patient Stories Search Page
- Annual Mammogram Saves Breast Cancer Survivor's Life
August 13, 2019
Angelique Nedved started giving herself an annual birthday gift when she turned 40 – a breast cancer screening mammogram. “I have a February birthday, so I scheduled my mammogram for February and always considered it my gift to myself and to my family,” she says.
Although some women are afraid to have screening mammography, Angelique contends this is flawed logic. “If you want to be around for a long time, then do your due diligence and get screened,” she says. “Breast cancer isn’t necessarily the big, scary monster it used to be. If you get out ahead of it, you have a lot better chance of overcoming it and enjoying a lot more birthdays.”
Marc Hoffmann, MD, Angelique’s medical oncologist at The University of Kansas Cancer Center, agrees that mammograms are important, and adds that his colleagues in radiology who specialize in interpreting mammography detect early breast cancers at a rate that exceeds the national average.
“Our team focuses solely on breast cancer diagnosis and treatment,” he says. “It makes a difference in outcomes because this is all we do. Our radiologists specialize in reading mammograms every single day and know exactly what they’re looking at.”
Second opinion, definitive answers
Angelique’s case didn’t start with such a clear mammogram reading, however. When she was 45, in February 2016, Angelique noticed a hard, pea-sized lump in her breast and pointed it out during her regular mammogram at a Kansas City area healthcare facility. A follow-up ultrasound indicated a clogged gland, and she was told to follow up again in 6 months. But instead of resolving, Angelique noticed the lump enlarging.
By August, Angelique and her family had moved and she chose a primary care physician closer to her new home in Kansas City, Kansas. A routine exam to establish herself as a patient with her new doctor resulted in a referral to The University of Kansas Health System to have the lump assessed by breast care specialists. Within 3 days, Angelique had an appointment at The University of Kansas Cancer Center, and 2 days after that, she received the news that her “clogged gland” was a tumor.
“It all went so fast once I got to the cancer center,” says Angelique, who has no family history of breast cancer. “And after the doctors there saw me, they said there was no question that it was cancer.”
In fact, Angelique’s cancer was quite advanced. “Her cancer was diagnosed as triple-negative, an aggressive type of cancer, and stage 3C, which is as close to metastatic as possible before spreading,” Dr. Hoffmann notes. “The goal at that point was to establish control of her cancer with systemic treatment.” In other words, Angelique needed strong chemotherapy to flood her system, destroying any cancer cells that were moving beyond her breast.
Aggressive breast cancer treatment, positive results
Like many breast cancer patients, Angelique’s first reaction was, “Let’s get rid of my breasts right now,” she recalls. However, the standard of care for her type of breast cancer involves leaving the tumor in place during chemotherapy. “The actual breast tumor and lymph nodes are surrogates, indicating how well the treatment is working throughout the body,” Dr. Hoffmann says.
Due to the type of cancer she had, Angelique also entered a clinical trial. Dr. Hoffmann notes this is another benefit of seeking treatment at a National Cancer Institute-designated cancer center within an academic health system. Research provides crucial data that may result in important medical advances. Angelique was the 32nd patient to enroll in a cohort of 100, and researchers randomly assigned her to the control group, meaning her care followed current standards without any experimental interventions.
Within 2 weeks of diagnosis, Angelique had her first chemotherapy treatment. “In those 2 weeks, I was researching and learning about my cancer,” she says, adding that she also received genetic testing following her diagnosis. “I felt empowered when I had facts, and my doctors were wonderful in providing accurate and understandable information and guiding me to the best sources. My biggest concern was whether my cancer would respond to the chemotherapy.”
It did. During her chemotherapy, Angelique could feel her tumor shrinking, giving her hope. After 16 treatments, she was ready to schedule surgery and opted for a bilateral (double) mastectomy. Dr. Hoffmann notes that Angelique is among an increasing number of women who choose to have all their breast tissue removed. The decision is always based on conversations between the patient and medical team, considering the pros and cons of this aggressive approach.
More rarely, women in Angelique’s situation question the need for mastectomy at all. “If they respond well to chemotherapy and the tumor disappears completely, they may ask why they need to have surgery,” Dr. Hoffmann says. “The truth is, we don’t know for sure whether surgery improves outcomes in these cases, but the current standard of care for this type of breast cancer is to follow chemotherapy with surgery even when the response to chemo is complete, as in Angelique’s case. Until there is compelling data to indicate otherwise, we will recommend this standard.”
Christa Balanoff, MD, a breast surgical oncologist with The University of Kansas Cancer Center, performed Angelique’s bilateral mastectomy on January 30, 2017, and Angelique waited anxiously for the follow-up pathology results. On February 2, she got the call. “There was no cancer present in my tissue or lymph nodes. It was amazing news,” she says.
Despite the good news, Angelique still needed to complete her treatment regimen with radiation therapy, which was performed at The University of Kansas Cancer Center. Dr. Hoffmann notes that another clinical trial is underway exploring whether patients who have early-stage breast cancer, with no evidence of disease in their lymph nodes after surgery, necessarily need radiation therapy. However, Angelique’s cancer was so advanced when she was diagnosed, there was no question that radiation would be recommended.
For 31 days in March and April 2017, Angelique received a 2-minute zap of highly targeted radiation. The painless procedure caused what she describes as a “minor sunburn” on her skin and created some localized skin tightening. Yet those minor side effects did not stop her reconstructive surgery with plastic surgeon Eric Lai, MD, in October. “I’m really pleased with the results,” she says. “The surgical team was very specialized and did a phenomenal job.”
Specialized, collaborative breast cancer care
Throughout her diagnostic and treatment journey at The University of Kansas Cancer Center, Angelique says she felt cared for by a supportive, collaborative team. “It was just a very thoughtful package in the way the doctors collaborated together and coordinated my care. The tools and resources they provided were very helpful,” she notes.
She was especially impressed with the mobile app she used, which was made possible by Uhlig LLC – a Kansas City-based technology company – to manage her care. From her smartphone she made appointments, accessed billing information and medical records, and interacted with her care team.
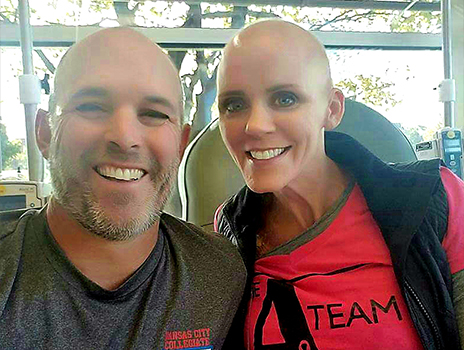
Anyone who meets Angelique today sees no evidence of her recent treatment journey, and her prognosis is good. “The odds are definitely in her favor,” Dr. Hoffmann says. And both he and Angelique remain staunch advocates of regular screening exams.
“I don’t know if we would have picked up her cancer sooner had we done the initial screening mammogram ̶ that would just be speculation,” he says. “But I do know that going somewhere highly specialized can make a difference, being willing to participate in a clinical trial leads to better care for more people and having a positive, open attitude can make things easier. We really work to support all of our patients with these important aspects of care.”
Your first choice for a second opinion.
Having confidence in your diagnosis and treatment is critical when you're faced with the possibility of cancer. Call 913-588-1227 for a second opinion.
This individual participated in a clinical trial of an investigational treatment. Clinical trials are different from standard medical care. As with all research studies, clinical trial participant outcomes vary. Before participating in a clinical trial, it is important to discuss the risks and benefits with your healthcare provider.